and practical tips as we emerge…
Just over one year into the pandemic, we have grown accustomed to working from home, staying in, and doing less, but how has this affected our cardiovascular risk? Dr Scott Murray, consultant cardiologist at Wirral University Teaching Hospital, outlines seven ways to combat heart disease in a pandemic.
- Avoid comfort foods
The past year has been very difficult for almost everyone. One of the ways many of us, including myself (!) deal with boredom, frustration and uncertainty is to consume more comfort foods. These products are generally high in processed carbohydrates and fats, salt, and sugar. When we eat more comfort food, this can and often does, raise our insulin levels. When your insulin levels are over-stimulated this can lead to a rise in certain types of cholesterol. For some people, their body is able to deal with this over-production and there may not be any long-term harm done. However, for other people, certain elements of these cholesterols, can end up inflaming the artery walls which can ultimately lead to a heart attack or heart disease.
2. Try intermittent fasting *disclaimer*
It isn’t necessarily a popular recommendation but there could be real benefit in intermittent fasting for some people. Try missing a meal or closing your ‘eating window’ to six hours. This will take the pressure off your fat cells and have a positive impact on your metabolic health which can improve your cardiovascular risk. For more information on intermittent fasting and advice for people thinking about trying this for the first time click here.
3. Make sure you stay active
It isn’t rocket science, physical activity improves heart health. Try to do something every day that gets you moving. One of the best kinds of exercise for heart health is high intensity interval training or HIIT. However, this may not be possible for everyone. If you take a lot of calls for work, why not make them whilst walking round the house or better still, the block.
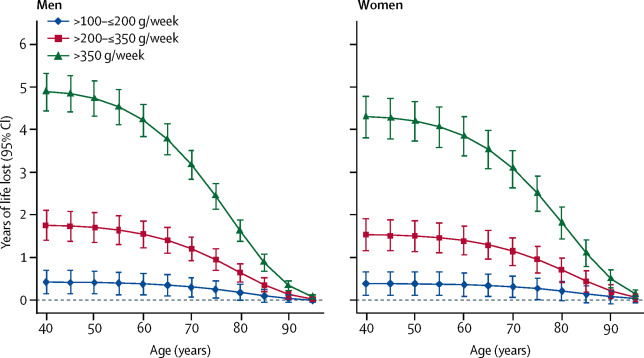
4. Have alcohol free days
Research carried out in 2020 has shown that at least one in five of us increased our alcohol consumption last year. Habits form quickly and can be hard to break. NHS advice recommends drinking no more than 14 units of alcohol per week and this should be spread over three or more nights. This is the same as nine 125ml glasses of average strength wine or seven medium strength beers. Using the graph below, the Lancet explains risk thresholds for alcohol consumption. As you can see, the highest risk is attributed to men in their 40s who consume 350g and over, or 18 glasses of wine or pints of beer per week. In addition, a 40-year-old regularly drinking between 200g and 350g of alcohol per week – about 10 to 18 glasses of wine or pints of beer, will have a reduced life expectancy of around one to two years.
There are several other risks associated with drinking including, poor decision making, a blood pressure spike the day after drinking and a weakened immune system. All of these are risk factors for cardiovascular disease.
5. Turn your email off (or better still take it off your phone so you do not look at them in non-work hours.)
Stress is a big contributor to high blood pressure which is bad for your heart. For many it can be hard to switch off from work. Often there is little or no separation between work and home and we can find ourselves checking our emails or work WhatsApp messages well into the evening or even in the middle of the night. When you don’t switch off from work you are less productive and less creative but more worryingly your stress levels go up, increasing cortisol levels. This can increase blood cholesterol, triglycerides, blood sugar, and blood pressure. These are common risk factors for heart disease.
6. Don’t snack
When we have regular snacks throughout the day, on top of meals, our blood sugar levels can spike, sometimes four or five times per day. This can negatively impact on how your kidneys manage your blood pressure. High blood pressure can also be detrimental to heart health. Stop snacking, instead, get outside, get moving, go for a walk or a run. Any amount of physical activity is good for your heart.
7. Feed your gut
We need to give our gut plenty of nutrients and fibre. Fibre is found in foods such as whole grains, whole wheat, beans, whole nuts and vegetables such as carrots and celery. Food which is high in fibre tends to fill you up more, so you feel less hungry and are hopefully less likely to snack on processed sugary foods. Fibre can also lower cholesterol and blood pressure, again helping prevent heart disease. When we have a diet that is high in fibre, it causes the part of the cell that converts food to energy to spring into action, improving your metabolic rate. Better metabolism = better heart health.
Has COVID been bad news for your heart?
Dr Scott Murray said:
“In short, yes. Many more of us have a more sedentary lifestyle. People are worried to go out. Those that have had COVID may feel too anxious (or tired) to start exercising again. It has promoted a new way of thinking ‘stay at home and everything will be ok’ and whilst that was necessary for a period, it is important that we get back to an active lifestyle. The impact of long COVID is still unknown, approximately one in ten of us continues to experience symptoms of COVID beyond 12 weeks.”
If you know that you have fallen foul of one of the above and you perhaps have a family history of heart disease, then you’re certainly increasing your cardiovascular risk and it might be time to think about putting some new habits in place.
Practical tips as we come out of lockdown
As we begin to emerge from what has been a year of staying at home, we need to spring back into action to protect our heart health.
- Get outside – enjoy some lovely sunshine and get some well needed vitamin D.
- Get moving – try to work off some of those lockdown pounds!
- Sleep better – create good sleep habits
- Reconnect with friends
Heart disease is not contagious in the same way Covid-19 has proved to be, but it is certainly as deadly. Heart and circulatory disease account for over one quarter of all deaths in the United Kingdom: one death every three minutes. Forty-four thousand people under the age of 75 will die from heart disease every year and the North West has one of the highest rates in the country. The only way to get an accurate picture of your heart health is to have a scan of your heart. In the same way women routinely have a mammogram, we want heart tests to be routinely available, accessible and affordable to those that need them.
If you feel concerned about your heart health and you would like to book a consultation with one of our consultant cardiologists, please register your interest here. The clinic is currently being fitted out to the very highest specification, ready to receive patients in the Spring.
*Disclaimer*
While intermittent fasting has many proven benefits, it can be dangerous for some people, particularly for those who are taking medication – where doses may need to be changed. A big change in diet can also activate gallstones that previously existed but were dormant.
Discuss any medication and relevant lifestyle changes with your doctor before fasting. Those who should NOT fast include:
- Those who are underweight or have a BMI lower than 18.5
- Those with an eating disorder such as anorexia
- Pregnant and breastfeeding women
- Anyone under the age of 18
- Those with type 1 diabetes or type 2 diabetes on insulin
We are currently offering 10% of all consultations, please register here and use the code 10%Off to benefit from the discount.