What is plaque, why does it build up in your arteries and how can you stop it?
Deposits of particular particles that carry cholesterol (and are made in the liver) can change and accumulate in your arteries. This build-up can lead to harmful inflammation. The body recognises this and sends cells to repair the problem and ‘contain’ the deposit. These cells create a seal over the inflamed deposit. Over time this ‘arterial pimple’ becomes a mature ‘plaque’. This process is known as atherosclerosis. Eventually, plaque can collect to such an extent that it calcifies, hardening and blocking the artery slowly, over years. This can lead to angina (lack of blood supply to the heart muscle). Sometimes a soft but hardening plaque can also rupture. When this happens a blood clot can form on top of the split plaque, this can cause a fatal blockage, a heart attack.
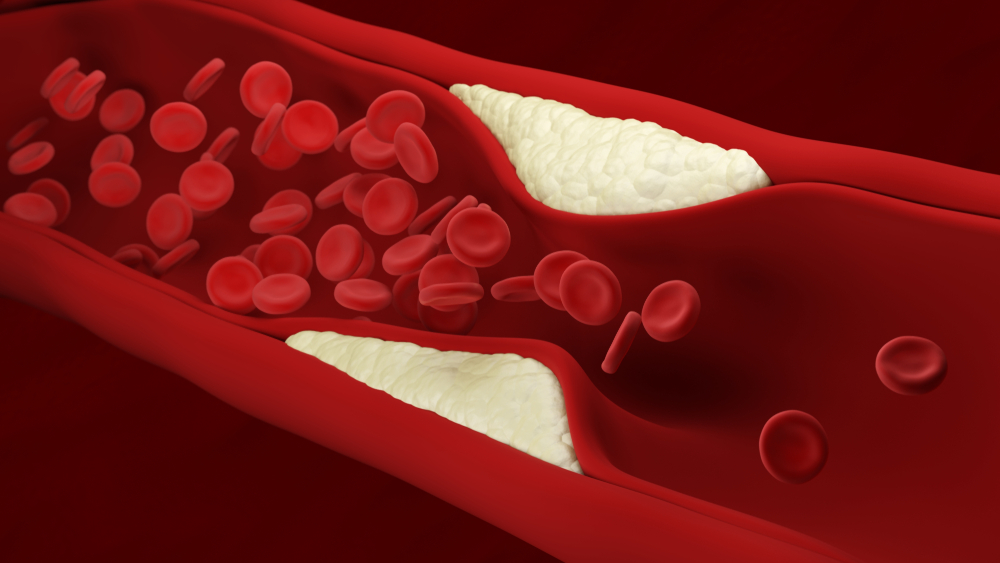
Atherosclerosis. Plaque building up inside an artery
Why does it build up in your arteries?
Inflamed collections of plaque can build for many reasons including, genetic predisposition, poor diet, lack of exercise, smoking, stress, poor sleep or related risks such as diabetes, high cholesterol and high blood pressure. Having a pre-existing inflammatory condition can also accelerate plaque growth, due to revved up inflammation signalling. So conditions such as Psoriasis, Rheumatoid Arthritis, HIV, Autoimmune disease, Kidney Failure, erectile dysfunction can all give hints that heart plaque is more likely.
Can you stop it?
This depends on its stage of development.
The first stage in plaque development is called the ‘fatty streak’. This can be one of the ways that the body heals. Cholesterol and proteins go to the site of inflammation or injury, possibly as part of the immune function. By the age of 20-30, most people have some fatty streaks within their arteries. They are not dangerous and can even diminish over time. The problem only comes when the damage is continuous and these agents get trapped there and cannot be ‘reversed’ out. This is worsened if you smoke, have high blood pressure and have a diet high in sugar and bad fats. Failing to exercise (to keep arterial walls healthy and happy) also can accelerate the damage.
The second stage of plaque development is called ‘plaque progression’ when the damage is established and the inflammatory reaction is in full swing with the body engaged in an internal war between inflammation and clotting verses anti-inflammatory and blood thinning. If the body cannot find a solution to the extrinsic system damage, that is occurring minute by minute, hour by hour, then it often decides to try and shut down the plaque by drafting in the cells that can thicken or ‘cement’ the soft plaque with more fibrous or calcified tissue components.
The third and final stage is known as ‘plaque disruption’. This is when the plaque has accumulated to such an extent that it becomes the pathological entity of atherosclerosis. Atherosclerotic plaque can be a mixed bag of soft and tough components all together in a ‘yolk like’ bleb. If the plaque grows and becomes under so much intra-plaque pressure, coupled with external shearing forces from blood pressure, then the junctions of soft and hard components can de-bond (like an ice-lake shattering)

releasing the soft components below and exposing them to the blood which causes a clot. At this point athero-sclerosis becomes athero-thrombosis and an Acute Coronary Syndrome (ACS) or ‘heart attack’ occurs. This needs hospital admission for medication and the possibility of a procedure such as a stent or bypass operation.
Removing plaque from the artery walls in the late stages is very difficult and often needs palliating with invasive treatment such as a stent. Certain medications, such as statins or aspirin can be very effective in reducing further accumulation of atherothrombosis. Statins lower the amount of cholesterol known as low-density lipoprotein or LDL that your body makes and help reduce inflammation and many other things, ultimately reducing your risk of heart attack, heart disease and stroke.
Although it is difficult (but not impossible!) to remove plaque that is already there, the main things we want to achieve are to stop the high blood pressure, blood sugar, smoking and inflammation that is ‘driving the bus’ to prevent the progression of plaque. Regression can happen as a bonus too – see this latest paper here.
We have summarised some of the key lifestyle factors that will reduce your risk of heart disease here:
Maintain a healthy diet
Making sure you have a diet that is high in lean protein, fibre and good fats (omega 3) such as oily fish, nuts, eggs (the only vitamin not in an egg is Vit C!), extra virgin olive oil and avocado. Reducing or eliminating your intake of processed, package food is paramount. Eliminating sugar and profoundly starchy, high glycaemic index (GI) carbohydrates is important. Green leafy vegetables help the body to make nitric oxide (a chemical vital to artery health). Fresh fruit and above ground vegetables give further vitamins, fibre and nutrients. In some people, the supplementation of Vitamin D, Magnesium and Vit K2 makes theoretical sense but currently has no supportive data.
Exercise
The government recommends 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity a week for optimal health. Get it however you can, walking is enough to start with and to build a base. Try to take your muscle groups to failure though using light weights or calisthenics type work – think “Joe Wicks type” short blasts of high intensity activity. Remember that you can’t out exercise a bad lifestyle and that occasionally exercise on a bad lifestyle is detrimental and pro-inflammatory. A recent study demonstrated how lifestyle interventions including diet and exercise can make a big difference to coronary artery disease. Read our review of the study here to understand how Venturi can help you to make these changes.
Smoking
It is a well proven fact that smoking is bad for you and can lead to heart disease. Quitting smoking is the single best thing you can do to reduce your risk. Try the NCST very brief advice website as a starter.
Stress and sleep
High levels of stress or poor or insufficient sleep do not lead directly to heart disease. However, they are often linked to poor decision making. When we feel tired or stressed, we often comfort eat, drink too much alcohol and exercise less. Stress can also raise your blood pressure and body inflammation. Over time high blood pressure and inflammation damage your heart and increase your risk of coronary heart disease.
Inherited problems
Some heart conditions are hereditary. If a first degree relative i.e. someone in your immediate family – you mum, dad or one of your siblings, has died from a heart related problem before the age of 75, this may increase your risk. It is always worth knowing your family history and having your heart scanned if you feel you may be at risk. Check out one of our other blogs – Heart disease: does it run in the family, for more information on this subject.
In conclusion, whilst it can be difficult to remove plaque once it is already there, it is not impossible. There are plenty of steps you can take to settle it down from hot to cold and halt its progression. If you would like more expert advice and information about heart screening and correctly calculating your risk of heart disease please get in touch here